Are Peas Low FODMAP? The Complete Guide for IBS

If you're managing IBS symptoms and wondering about peas, you're asking the right question. Peas are conditionally low FODMAP – meaning they're gentle on digestion in smaller servings but can trigger symptoms when you eat too much. This nuanced answer is exactly why understanding the low FODMAP diet matters so much for the nearly 1 billion people worldwide living with IBS.
Key Takeaways
- Peas are low FODMAP in small servings, such as up to 53g of canned green peas.
- Larger portions of peas contain high levels of galacto-oligosaccharides (GOS) that can trigger IBS symptoms.
- Portion control is essential for people following a low FODMAP diet when consuming peas.
- Peas are considered conditionally low FODMAP because their impact depends on the serving size.
- Understanding the low FODMAP diet is important for managing IBS symptoms effectively.
Table of Contents
At Gourmend Foods, we know how frustrating it can be to navigate which foods work for your gut and which don't. That's why we're breaking down everything you need to know about peas and FODMAPs, plus the bigger picture of how this science-backed approach can help you eat confidently again. For more foundational information, visit our FODMAP blog for in-depth guides and updates.
Understanding the Low FODMAP Diet
Before we dive into the specifics of peas, let's establish what we're working with. The low FODMAP diet isn't just another food trend – it's a clinically proven approach for managing digestive symptoms, particularly for people with IBS. For a broader overview, you can also explore our Learn blog for more about digestive health and dietary strategies.
What is the Low FODMAP Diet?
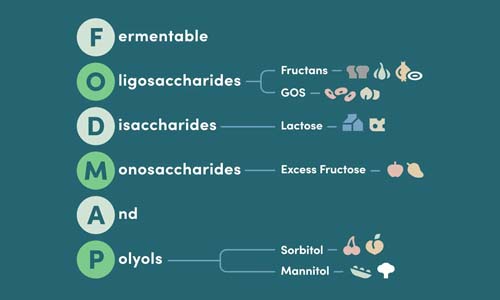
FODMAP stands for: Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols – types of carbohydrates that can be poorly absorbed in the small intestine.
Here's how it works: when these carbohydrates aren't properly absorbed, they travel to your large intestine where gut bacteria ferment them. This fermentation process produces gas and draws water into the bowel, leading to the uncomfortable symptoms many of us know too well – bloating, gas, abdominal pain, and changes in bowel habits. For a detailed breakdown of high and low FODMAP foods, see this Monash University resource.
The low FODMAP diet involves a structured three-phase approach:
- Elimination Phase: Remove high FODMAP foods for 4-6 weeks
- Reintroduction Phase: Gradually test foods one at a time to identify personal triggers
- Personalization Phase: Create a long-term eating plan that avoids only your specific problem foods
Important Note: While we share evidence-based information about the low FODMAP diet, this approach should be followed under the guidance of a registered dietitian or healthcare provider, especially during the elimination phase, to ensure nutritional adequacy.
Who Should Follow the Low FODMAP Diet?
The low FODMAP diet isn't for everyone. Research shows it's most beneficial for:
- People diagnosed with IBS: Studies indicate that 70-80% of people with IBS see symptom improvement on a low FODMAP diet
- Individuals with other digestive disorders: Some people with inflammatory bowel disease (IBD) or functional dyspepsia may also benefit
- Those experiencing unexplained digestive symptoms: Under medical supervision, it can help identify trigger foods
However, this diet is not recommended for general weight loss or as a long-term restrictive eating plan. It's a therapeutic tool designed to identify and manage specific digestive triggers.
Symptoms and Causes of IBS

Understanding IBS helps explain why the low FODMAP approach works so well. With two-thirds of Americans reporting digestive issues, recognizing these patterns is more important than ever.
Common Symptoms
IBS symptoms can vary significantly from person to person, but the most common include:
- Abdominal Pain and Cramping
- Often the most disruptive symptom, typically improving after bowel movements
- Bloating and Gas
- Can cause visible abdominal distension and significant discomfort throughout the day
- Altered Bowel Habits
- Including diarrhea (IBS-D), constipation (IBS-C), or alternating between both (IBS-M)
These symptoms often occur together and can significantly impact daily life, work productivity, and social activities. The unpredictable nature of IBS is often as challenging as the physical symptoms themselves.
Factors Influencing IBS
IBS isn't caused by a single factor. Instead, it's influenced by a complex interaction of:
- Dietary triggers: Including high FODMAP foods, fatty foods, caffeine, and alcohol
- Stress and psychological factors: The gut-brain connection means emotional stress directly impacts digestive function
- Gut microbiome imbalances: Changes in beneficial bacteria can affect digestion and symptom severity
- Food sensitivities: Beyond FODMAPs, some people have triggers like gluten or specific food additives
This is exactly why we created Gourmend Foods – to provide clean, organic, low FODMAP alternatives that remove the guesswork from cooking. Our broths and seasonings use ingredients like chives and scallion greens instead of onions, and garlic chives instead of garlic bulbs, so you can enjoy rich, gourmet flavors without digestive distress.
FODMAP Food Groups: What to Know
To understand why peas fall into a gray area, let's break down the different types of FODMAPs and where they're commonly found.
Types of FODMAPs
- Fructans
- Found in garlic, onions, wheat, and many processed foods
- Excess Fructose
- Present in certain fruits like apples, pears, and honey
- Galacto-oligosaccharides (GOS)
- Found in legumes like beans, lentils, and yes – peas
- Lactose
- The sugar in dairy products
- Polyols
- Found in stone fruits and sugar alcohols like sorbitol and xylitol
Peas are primarily high in GOS, which is why portion size becomes so critical. In small amounts, the GOS in peas can actually act as beneficial prebiotics, feeding the good bacteria in your gut. But in larger servings, they can overwhelm your digestive system's ability to process them comfortably.
You might be wondering: "If GOS feeds good bacteria, why avoid it?" The answer is timing and amount. During the elimination phase of a low FODMAP diet, you're giving your gut a break from fermentation to reduce symptoms. Once you've identified your triggers and your symptoms are under control, you can strategically reintroduce prebiotic foods like peas in amounts that work for your body.
Low and High FODMAP Foods

Understanding which foods fit where on the FODMAP spectrum helps you make confident choices in the kitchen. Here's a comprehensive breakdown of the foods that support easier digestion versus those that commonly trigger symptoms. For more inspiration, browse our Low FODMAP Recipes blog for practical meal ideas.
Quick Reference: Green vegetables like spinach, carrots, and zucchini are typically low FODMAP, while garlic, onions, and most legumes (including peas in large amounts) are high FODMAP.
Low FODMAP Vegetables
These vegetables form the foundation of gut-friendly cooking:
- Leafy greens: Spinach, arugula, lettuce, and kale
- Root vegetables: Carrots, potatoes, parsnips, and turnips
- Squash family: Zucchini, yellow squash, and pumpkin
- Other favorites: Green beans, cucumber, tomatoes, and bell peppers
Notice what's missing from typical cooking bases? Onions and garlic – the biggest culprits for digestive distress. This is why we use chives, scallion greens, and leek tops in our Gourmend broths instead.
High FODMAP Vegetables to Watch
These vegetables can trigger symptoms, especially in larger portions:
- Allium family
- Garlic, onions, shallots, and the white parts of leeks and scallions
- Cruciferous vegetables
- Cauliflower, Brussels sprouts, and cabbage in large amounts
- Legumes and pods
- Fresh peas, sugar snap peas, and most beans
- Mushrooms
- Most varieties, though oyster mushrooms (like those in our broths) are lower FODMAP
Where Peas Fit In
Here's where it gets interesting with peas specifically:
| Pea Type | Low FODMAP Serving | High FODMAP Threshold |
|---|---|---|
| Canned green peas (drained) | Up to 53g (about 1/4 cup) | Over 75g |
| Frozen green peas | Up to 33g (about 2 tablespoons) | Over 65g |
| Sugar snap peas | Up to 5 pods | Over 10 pods |
| Snow peas | Up to 10 pods | Over 15 pods |
Serving Size Matters: The difference between a gut-friendly meal and digestive discomfort often comes down to portions. This is why measuring matters during the elimination phase.
Other Food Categories
Beyond vegetables, understanding FODMAPs across all food groups helps you build complete, satisfying meals:
Low FODMAP Staples:
- Grains: Rice, quinoa, oats, and sourdough spelt bread
- Proteins: Plain meats, poultry, seafood, and eggs
- Fruits: Oranges, kiwi, pineapple, and berries (in moderation)
- Dairy alternatives: Lactose-free milk, almond milk, and hard cheeses
High FODMAP Foods to Limit:
- Grains: Wheat bread, regular pasta, and barley
- Fruits: Apples, pears, stone fruits, and dried fruits
- Legumes: Most beans, lentils, and chickpeas
- Sweeteners: Honey, agave, and sugar alcohols
Focus on Peas: Are They Low FODMAP?
Now let's get specific about peas and what makes them tricky to categorize. For a scientific perspective on pea protein and FODMAPs, see this Monash University article.
Understanding Peas and FODMAPs
Peas contain primarily galacto-oligosaccharides (GOS), a type of FODMAP that serves a dual purpose in your digestive system. In small amounts, GOS acts as a prebiotic, feeding beneficial gut bacteria and supporting overall gut health. However, when you consume larger portions, these same compounds can overwhelm your digestive system's ability to process them comfortably.
You might be wondering: "Why are peas sometimes okay and sometimes not?" The answer lies in your gut's processing capacity. Everyone has a different threshold for FODMAPs, and peas sit right at that threshold for many people.
Research shows that the fermentation of GOS in peas produces gas and can draw water into the intestines, leading to the bloating, cramping, and altered bowel habits characteristic of IBS symptoms. This is why portion control becomes so critical with peas.
Serving Size Considerations for Peas
The key to including peas in a low FODMAP diet is understanding exactly how much you can tolerate:
Canned Green Peas: These are your most generous option at up to 53g drained weight (roughly 1/4 cup). The canning process may reduce some FODMAP content, making them more tolerable.
For frozen peas, the threshold is lower – about 33g or roughly 2 tablespoons. Fresh peas fall somewhere in between, but individual tolerance varies significantly.
During IBS Flares: Even low FODMAP portions of peas might be too much when you're experiencing active symptoms. This is when focusing on the gentlest foods – like our organic bone broths – can help settle your system. For a comforting meal idea, try our Low FODMAP Braised Short Ribs recipe that pairs well with gentle sides.
Practical Strategies for Including Peas
If you love peas and want to include them in your low FODMAP journey, here are evidence-based approaches:
- Start small: Begin with just 1 tablespoon and monitor your response
- Choose canned over frozen: The processing may make them more digestible
- Pair with low FODMAP foods: Don't combine peas with other borderline foods in the same meal
- Time it right: Include peas when your symptoms are well-controlled, not during flares
Remember, the goal isn't to avoid peas forever – it's to understand your personal tolerance and enjoy them in amounts that work for your body. This individualized approach is what makes the low FODMAP diet so effective for long-term symptom management.
How to Follow the Low FODMAP Diet

Successfully navigating the low FODMAP diet requires a structured approach. Here's how to implement it effectively while maintaining nutritional balance and culinary enjoyment.
The 3-Step Approach
The low FODMAP diet isn't meant to be restrictive forever. It's a systematic process designed to identify your specific triggers:
Phase 1: Elimination (4-6 weeks)
Remove all high FODMAP foods from your diet while focusing on confirmed low FODMAP options. This phase gives your digestive system a break and establishes a symptom baseline.
Phase 2: Reintroduction (6-10 weeks)
Systematically test one FODMAP group at a time – including peas as part of the GOS group. Start with small amounts and gradually increase while monitoring symptoms.
Phase 3: Personalization (Ongoing)
Create your individualized long-term eating plan based on what you've learned about your triggers and tolerances.
Practical Tips for Success
Based on our experience helping thousands of customers navigate gut-friendly cooking, here are the strategies that make the biggest difference:
- Keep detailed food and symptom logs: Track not just what you eat, but when, how much, and how you feel 2-4 hours later
- Read labels religiously: High FODMAP ingredients hide in unexpected places – garlic and onion powders are everywhere
- Invest in quality low FODMAP staples: Products like our organic broths eliminate guesswork and provide reliable flavor bases
- Plan meals in advance: Having low FODMAP options ready prevents impulsive food choices that might trigger symptoms
Essential Tool: Use the Monash University FODMAP app – it's the gold standard for portion guidance and is regularly updated with new research.
Additional Considerations
Successfully managing IBS with the low FODMAP diet extends beyond just food choices. Here are the critical factors that can make or break your long-term success.
Maintaining Nutritional Balance
The restrictive nature of the elimination phase raises important nutritional concerns that we see our customers navigate regularly:
Fiber Intake: Removing high FODMAP fruits, vegetables, and grains can significantly reduce your fiber intake. Focus on low FODMAP fiber sources like carrots, zucchini, and oats to maintain digestive health.
Calcium presents another challenge when limiting dairy products. While lactose-free dairy and fortified plant milks help bridge this gap, working with a registered dietitian ensures you're meeting all micronutrient needs during the restrictive phases.
- Protein diversity: Plain meats, eggs, and firm tofu provide complete proteins without FODMAP concerns
- B-vitamin support: Fortified rice milk and nutritional yeast help replace nutrients typically found in wheat products
- Prebiotic balance: Small amounts of low FODMAP foods like peas (within tolerance) help maintain beneficial gut bacteria
This is where quality products become essential. Our organic broths provide concentrated nutrition and flavor without the guesswork – giving you confidence that you're nourishing your body while managing symptoms.
Lifestyle Modifications That Matter
Research consistently shows that IBS management requires addressing the gut-brain connection alongside dietary changes:
- Stress Management Techniques
- Regular meditation, yoga, or deep breathing exercises can significantly reduce symptom severity. The vagus nerve directly connects your brain to your digestive system, making stress management crucial for gut health.
- Physical Activity
- Gentle, regular exercise promotes healthy gut motility and reduces stress hormones. Even a 20-minute daily walk can improve digestive function.
- Sleep Quality
- Poor sleep disrupts gut bacteria balance and increases inflammation. Aim for 7-9 hours of consistent, quality sleep to support your digestive healing.
The 80/20 Rule: Many of our customers find that dietary changes account for about 80% of their symptom improvement, while stress management and lifestyle factors contribute the remaining 20% – but that 20% often determines long-term success.
When to Seek Professional Support
While the low FODMAP diet is highly effective, certain situations require immediate medical attention:
You should contact your healthcare provider immediately if you experience blood in your stool, unexplained weight loss, severe abdominal pain, or symptoms that worsen despite dietary changes.
Additionally, consider professional guidance if:
- You're struggling to identify trigger foods after completing reintroduction phases
- Your symptoms significantly impact your quality of life or mental health
- You're concerned about nutritional adequacy during the elimination phase
- You have other medical conditions that complicate dietary management
Bringing It All Together
The question "are peas low FODMAP?" perfectly illustrates why the low FODMAP diet requires nuance rather than simple yes-or-no answers. Peas can be part of a gut-friendly diet when consumed in appropriate portions – up to 53g for canned varieties or about 2 tablespoons for frozen peas.
Success with the low FODMAP diet isn't about perfect restriction – it's about understanding your individual tolerance levels and making informed choices that support both your digestive comfort and nutritional needs.
The three-phase approach gives you the framework to systematically identify which foods, including peas, work for your unique digestive system. During the elimination phase, you'll likely avoid peas entirely. In reintroduction, you'll test your specific tolerance. And in personalization, you'll know exactly how to include them in your long-term eating plan.
Based on our experience supporting thousands of customers through their gut health journeys, we've learned that the most successful people focus on what they can eat rather than what they can't. This mindset shift transforms the low FODMAP diet from restrictive to empowering.
Remember that managing IBS effectively combines dietary strategies with stress management, regular physical activity, and professional support when needed. The low FODMAP diet provides the foundation, but lasting digestive wellness requires attention to your overall lifestyle and well-being.
Your Next Steps:
- Start with the elimination phase under professional guidance
- Keep detailed food and symptom logs
- Stock your pantry with certified low FODMAP staples
- Test peas during reintroduction, starting with small canned portions
- Focus on building a sustainable, personalized eating plan
With nearly 1 billion people worldwide living with IBS, you're not alone in this journey. The low FODMAP diet has helped countless individuals reclaim their relationship with food and significantly improve their quality of life. By understanding how foods like peas fit into this framework, you're taking an important step toward digestive wellness and culinary confidence.
Check out our Plant Based Bundle
Frequently Asked Questions
Are peas ok for IBS sufferers?
Peas can be tricky for IBS sufferers because they contain moderate amounts of FODMAPs. Small servings, like about 1/4 cup cooked green peas, are usually tolerated by many on a low FODMAP diet, but larger amounts may trigger symptoms. It’s best to test your personal tolerance and stick to smaller portions to enjoy peas without discomfort.
What green vegetables are low in FODMAP?
Several green vegetables are low in FODMAPs and great for digestive comfort, including spinach, kale, green beans, bok choy, and the green parts of scallions and leeks. These veggies offer fresh, vibrant flavors and nutrients without the digestive downside of high-FODMAP options like asparagus or broccoli.
What is a low FODMAP substitute for peas?
If you’re avoiding peas, try green beans or edamame in small amounts as a low FODMAP alternative. They provide a similar texture and fresh green taste without the fermentable carbs that can cause bloating or gas in sensitive guts.
What vegetables to avoid on FODMAP diet?
On a low FODMAP diet, it’s best to avoid high FODMAP vegetables like onions, garlic, cauliflower, mushrooms (except oyster mushrooms in moderation), asparagus, and certain beans and lentils in large amounts. These contain fermentable carbs that can cause digestive symptoms like bloating, gas, and discomfort.
What food calms an IBS flare-up?
Foods that are gentle on digestion, like bone broth, cooked low FODMAP vegetables, plain rice, and ripe bananas, can help calm an IBS flare-up. These foods are easy to digest, provide nutrients, and avoid common trigger ingredients, supporting your gut while you recover.
Is mayonnaise bad for IBS?
Mayonnaise itself is generally low FODMAP, as it’s mostly oil, egg, and vinegar or lemon juice. However, some commercial mayo brands may include garlic or onion powders, which can trigger IBS symptoms. Choosing clean-label, additive-free mayonnaise—or making your own with simple ingredients—is the best way to enjoy it without worry.