Co-authored by Laura Manning, MPH, RDN, CDN
The Low FODMAP Diet: The Complete Guide to Cooking, Eating & More
This is the ultimate guide to low-FODMAP eating and cooking. In this guide, you’ll learn:
- The basics of FODMAPs, including the foods that FODMAP-sensitive individuals should avoid
- How to prepare and eat meals that are nutritious and delicious after eliminating garlic, onions, and other ingredients from your diet
- The basics of smart shopping and flavorful cooking with low-FODMAP ingredients
If you're ready to learn how to follow a low-FODMAP diet for improved gut health, then you need to read this guide.
Let’s get started!
A diet that restricts high-FODMAP foods has been shown to minimize gastrointestinal symptoms for those with irritable bowel syndrome1 (IBS) and inflammatory bowel disease (IBD)2. In fact, research asserts that 50-80% of IBS sufferers that followed a diet low in FODMAPs found relief from their symptoms1.
The information in this guide is not intended to replace medical treatment and counsel that your health care provider offers. It is intended to educate and supplement personalized medical advice, while providing support at all stages of the low-FODMAP diet experience. Keep in mind that we offer these resources and suggestions for support, education and guidance only. Use them to complement consultations with a registered dietitian.
Part 1 FODMAP Basics
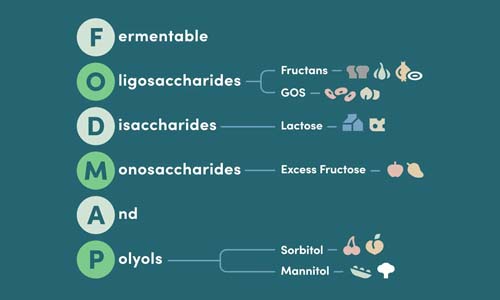
What does FODMAP stand for?
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols. These are short chain carbohydrates that are poorly absorbed in the small intestine, making them difficult to digest for many individuals.3
Found in many of the foods we eat every day, FODMAPs are not inherently unhealthy, so what makes them so troublesome to those with IBS or other digestive conditions?
FODMAPs are fermented in your gut during digestion, but if this happens too fast, abdominal cramps and other symptoms may occur.
During digestion, FODMAPs can draw excess water into the intestine, leading to stomach pain, diarrhea, and bloating.
Whether one or more of these FODMAP characteristics are at play will depend upon on the amount consumed and an individual's degree of intolerance of the carbohydrates.
It’s important to work with a registered dietitian or nutritionist if you suspect that you have a FODMAP sensitivity.
Here’s why:
- Your dietician can help you understand common FODMAPs like fructose and lactose
- They can assist you in determining your level of FODMAP tolerance
- They can help ensure you are getting necessary nutrients while limiting your intake of high-FODMAP foods
The most common FODMAPs include:
Oligosaccharides
Oligosaccharides are found in asparagus, beans, onions, garlic, and other food ingredients present in many American diets.
Fructans
Fructans, including barley, rye, wheat, asparagus, garlic and onions, are oligosaccharides. Some individuals with chronic digestive disorders may not digest them properly. They reach the large intestine undigested and are fermented by the guts beneficial bacteria.
Some fructans, such as inulin and chicory root, are often added to foods to give it more texture and fiber. These can add to digestive distress and it is important to look for these on a food label as it can increase the FODMAP content of a packaged food significantly.
Galactooligosaccharides (GOS)
A GOS is an oligosaccharide that is malabsorbed by everyone’s body to some extent, as our intestines lack the enzyme needed to break it down. When GOS' are fermented by the gut’s beneficial bacteria, gas is produced.
Individuals with IBS are often more sensitive to this reaction, experiencing stomach pain among other symptoms. High levels of GOS are found in legumes, so a diet that limits beans is often beneficial for those with a FODMAP sensitivity.
Disaccharides
Disaccharides are sugars found primarily in dairy products, but also in beer, sweet potatoes, and bread.
Lactose
A sugar composed of glucose and galactose, lactose is a disaccharide found in milk, curds, whey, dry milk solids, and other dairy products. The small intestine must produce sufficient amounts of the enzyme lactase in order to effectively digest lactose sugar.
If the body fails to produce enough lactase to digest lactose properly, then lactose intolerance will occur. Gastrointestinal distress can occur between 30 minutes to two hours after certain dairy products are consumed.4
There are several products that contain lactase which may help you better digest lactose. Available from most pharmacies, lactase tablets or drops are an enzyme supplement that may be helpful to some people who are lactose intolerant. Note that some of these supplements contain mannitol and other high-FODMAP polyols. Be sure to check the label and select a brand that is low FODMAP.
Monosaccharides
Monosaccharides are the simplest form of sugar and the most basic units of carbohydrates. The most common monosaccharide is fructose.
Fructose (in excess of glucose)
This monosaccharide is naturally found in honey, vine and tree fruits, asparagus and artichokes. Commercially, fructose is gleaned from maize, sugar cane, and sugar beets.
Often, this fruit sugar is added to food and drinks to enhance the taste. Additionally, fructose and glucose monosaccharides are combined to create high-fructose corn syrup.
Food containing fructose is considered low FODMAP if it has a less or equal level of fructose than glucose (like an unripe banana). Food that has more fructose than glucose (like an apple) is considered high FODMAP and is associated with digestive issues that occur when the body is unable to efficiently break down the sugar.
And Polyols
Polyols are found naturally in fruits and vegetables, and are frequently used as sweeteners in cough drops, medications, mints, and sugar-free gum.
When sugar polyols reach the large intestine for fermentation, these FODMAPs are frequently malabsorbed. The sugar polyols can pull water through the bowel or be fermented by intestinal bacteria, and these changes often result in discomfort.
The severity of symptoms will depend on the amount of polyols consumed, what other FODMAPs have been eaten that day, and if the gut was already in a sensitive state before introducing the polyols. The two most common polyols are:
Sorbitol
Sorbitols occur naturally in apricots, blackberries, cherries, nectarines, peaches, plums and prunes.
Mannitol
If you’re sensitive to mannitol, avoid cauliflower, celery, clingstone peaches, button mushrooms, snow peas, and watermelon.
The Takeaway:
FODMAPs include the fructose in fruits and vegetables, the galactans in legumes, the lactose in dairy products, the fructans in wheat, garlic, onion, and other foods, and the polyols in many fruits and vegetables.
For those who have trouble digesting FODMAPs, the carbohydrates end up reaching the colon, where they pull water into the intestine and are fermented by hydrogen-producing bacteria in the gut.
Part 2 Elimination, Reintroduction & Personalization
Following the low-FODMAP diet will help you understand the ways that different types of foods may act as a trigger for symptoms of IBS and overall digestive distress.
Your body’s reaction to FODMAPs will depend upon the type and amount you consume and your degree of intolerance to that fermentable carbohydrate.
Step 1: Adhere to a Low-FODMAP Diet for 2-6 Weeks
In this step, you should follow a diet that consists of balanced meals containing a variety of low-FODMAP foods within this format:
- Proteins: 5-6 ounces per day (a serving is: 1 ounce of fish, chicken, lean meats, firm tofu, 1 egg, ½ ounce of allowable nuts and seeds, ¼ cup of allowable beans)
- Whole grains and bread: 6-7 servings per day (a serving is 1 slice of gluten free bread, ½ cup of cooked grain (rice, quinoa) or gluten free pasta, 5 gluten free crackers or 1 small corn tortilla).
- Fruits: 2-3 servings per day (a serving is 1 medium whole fruit or 1 cup diced).
- Vegetables: 3-5 servings per day (a serving is ½ cup cooked or 1 cup raw).
- Dairy: 2 - 3 servings of low fat dairy per day (a serving is 1 cup of lactose-free milk or allowable non-dairy milk fortified with calcium and vitamin D, 1 cup of plain lactose-free yogurt or 1 ounce of aged cheese).
- Healthy fats: When possible, choose olive oil for cooking and for dressings.
The FODMAP content can vary among foods. It can be higher depending on the serving size and or ripeness. For example:
A honeydew melon is low FODMAP when eaten as a ½ cup serving, a moderate-FODMAP fruit at 2/3 of a cup and a high-FODMAP fruit at a 1 cup serving.
Bananas are low FODMAP when they are unripe and high FODMAP when they are ripe (when they have many brown spots).
*For specifics on quantities for most ingredients, keep reading and also check out the Monash University Low FODMAP app.
Here is an example of a low-FODMAP day, by meal:
Breakfast
- 1 cup cooked oatmeal
- 2 tablespoon 100% pure maple syrup
- 1 cup rice milk or lactose-free milk
- ½ ripe medium banana
- 1 hard-boiled egg
- ½ cup black coffee
Morning Snack
- 2 tablespoons peanut butter
2 brown rice cakes
Lunch
- 3 oz grilled chicken breast with olive oil over a bed of arugula lettuce and a small, sliced tomato
- 1 cup cooked quinoa, made with low FODMAP broth or water
- 1 cup cooked string beans
- 1-2 tablespoons olive oil, lemon juice, salt and pepper
Afternoon Snack
- 4 oz plain yogurt (Greek or lactose-free)
- 30 raspberries
Dinner
- 4 oz baked fish with lemon, herbs and olive oil
- 1 medium baked potato
- 1 teaspoon butter
- 1 cup sautéed kale in olive oil
Fluids
- Drink plenty of water. At least 8 cups a day.
Do your best to adhere to low-FODMAP portion sizes during the Elimination Phase, but allow yourself slight variations without added stress. Success will be achieved with careful planning and accurate information. Please note that:
- The Elimination Phase can take from 2 to 6 weeks to see a change in symptoms.
- If your symptoms have significantly decreased after 2 weeks, you can proceed to the Reintroduction Phase. Some people will need longer than others and this is normal as each person is different and has varying times to meet their goals.
- If after 6 weeks you have not seen a significant difference, it is advisable to contact your doctor to see if there is an underlying cause outside of diet.
Looking to make the FODMAP diet simpler? Our friends at ModifyHealth deliver delicious, fully-prepared, Low-FODMAP and gluten-free meals, expertly designed to help you quickly determine if FODMAPs are playing a role in your digestive symptoms. Simply visit ModifyHealth.com and enter code GOURMEND60 to save $20 off of your first 3 deliveries - $60 total savings, plus free nationwide shipping.
Step 2: Reintroduce FODMAPs Back Into Your Diet
This is where we can discover the most important information about your digestion: which FODMAPs cause you to have increased symptoms and how much of it acts as a trigger.
-
This phase can help you find out how food may affect you and how to have the least restrictive diet with your new knowledge. It is possible that your digestion can change over the years and you may need to re-challenge foods again.
-
The Reintroduction Phase can take between 6 to 8 weeks to complete. Start with one FODMAP group at a time and test one food in a gradual increase to a typical serving size over three days. This is a time where you may want to journal your experience and see what does and does not cause symptoms.
-
Once you have trialed one FODMAP group, begin eliminating foods from that group again and go on to the next group to test. This is to isolate one group at a time for best observations.
Here is an example of how to conduct a "reintroduction" (you are welcome to do this in any order that you like and/or choose different challenge ingredients).
Oligosaccharides (Fructans & GOS)
Select a food from the Fructan group and add to a meal every day for three days in a row. Then, do the same with a food from the GOS group.
Fructan Group Challenge: Using Garlic
Note: In the fructan group, it is suggested to challenge garlic, onions and wheat individually.
- Day 1: ¼ clove of garlic
- Day 2: ½ clove of garlic
- Day 3: 1 clove of garlic
- Later on Day 3: Any symptoms? If yes, then you are intolerant to fructans and should be cautious when eating foods in that group. If no, then you can continue to enjoy foods containing fructans in your regular diet, once all FODMAP groups have been challenged.
GOS Group Challenge: Using Pinto Beans
- Day 1: ¼ cup of pinto beans
- Day 2: ½ cup of pinto beans
- Day 3: 1 cup of pinto beans
- Later on Day 3: Any symptoms? If yes, then you are intolerant to GOS and should be cautious when eating foods in that group. If no, then you can continue to enjoy foods containing GOS in your regular diet, once all FODMAP groups have been challenged.
Disaccharides (Lactose)
Select a food in the Lactose group and add to a meal every day for three days in a row.
Lactose Group Challenge: Using Regular Cow’s Milk
- Day 1: ¼ cup regular cow’s milk
- Day 2: ½ cup regular cow’s milk
- Day 3: 1 cup regular cow’s milk
- Later on Day 3: Any symptoms? If yes, then you are intolerant to lactose and should be cautious when eating foods in that group. If no, then you can continue to enjoy foods containing lactose in your regular diet, once all FODMAP groups have been challenged.
Monosaccharides (Fructose)
Select a food in the Fructose group and add to a meal every day for three days in a row.
Fructose Group Challenge: Using Honey
- Day 1: ½ tablespoon honey
- Day 2: ¾ tablespoon honey
- Day 3: 1 tablespoon honey
- Later on Day 3: Any symptoms? If yes, then you are intolerant to fructose and should be cautious when eating foods in that group. If no, then you can continue to enjoy foods containing fructose in your regular diet, once all FODMAP groups have been challenged.
Polyols (Mannitol & Sorbitol)
Select a food from the Mannitol group and add to a meal every day for three days in a row. Then, do the same with a food from the Sorbitol group.
Mannitol Group Challenge: Using a Portobello Mushroom
- Day 1: ⅓ of a cooked Portobello mushroom added to dinner
- Day 2: ½ of a Portobello mushroom
- Day 3: 1 Portobello mushroom
- Later on Day 3: Check in with yourself to see if you have increased symptoms. If yes, then you are intolerant to mannitol and should be cautious when eating foods in that group. If no, then you can continue to enjoy foods from that group in your regular diet, once all FODMAP groups have been challenged.
Sorbitol Group Challenge: Using a Yellow Peach
- Day 1: ⅓ a cup of yellow peach
- Day 2: ⅔ cup of yellow peach
- Day 3: 1 medium yellow peach
- Later on Day 3: Any symptoms? If yes, then you are intolerant to sorbitol and should be cautious when eating foods in that group. If no, then you can continue to enjoy foods from that group in your regular diet, once all FODMAP groups have been challenged.
If at any time during the Reintroduction Phase, you begin to experience immediate symptoms and become uncomfortable, stop the challenge. Return to a strict low-FODMAP diet and give your body a rest for three days or until symptoms subside. Then you may start the next challenge.
Learning what your FODMAP triggers are can be very empowering. There is peace of mind that comes with having the information you need to best plan meals and the explanation you've wanted for why you may experience stomach trouble when eating certain foods.
Step 3: Personalize Your FODMAP Diet
- After you have challenged your FODMAP groups and determined which are your trigger foods, simply return to your regular diet and avoid those that you were sensitive to. For example, if garlic is your trigger, use garlic infused oils or garlic scape powder to flavor your recipes. If honey is your trigger, you can simply use 100% maple syrup in its place.
- Remember to follow a balanced meal plan that contains all the food groups and is adequate in fiber for good nutrition and optimal bowel health.
The Takeaway:
After you have completed the elimination diet and reviewed your findings with a doctor or dietician, you will be equipped with the insight you need to create a long-term, sustainable approach to avoiding FODMAPs associated with your personal symptoms, while resuming cooking and eating flavorful meals again.
Because we do not yet know the long term health effects of staying on a low-FODMAP diet, this diet is meant to be temporary to discover intolerances and not intended to be a long term eating plan.
Part 3 Onion, Garlic, and the Low-FODMAP Diet
In this chapter, we'll explain:
- What makes onion and garlic high-FODMAP foods
- If and when these can be consumed
- How to cook flavorful meals without using onion and garlic
Onions
All onions are considered high-FODMAP, and therefore have the potential to cause digestive distress.
Onions are a concentrated source of fructans, and it may be a difficult food to avoid while adhering to the low-FODMAP diet, as the bulb is frequently used to flavor an array of dishes.
The FODMAP content in onions can vary depending on the type of onion. One of the lowest concentrations of fructans is in Spanish onions, while shallots contain among the highest.
Unless you have found that fructans are not a problematic FODMAP for you, eliminate all onions while on the low-FODMAP diet.
This includes standard onions as well as:
- Shallots
- Onion powder
- Pickled onions
- The white bottoms of leeks and scallions
- Seasonings flavored with onion (in general, avoid spice mixes and blends, as dried garlic and onion are common ingredients in these).
Garlic
Like onions, fresh and dried garlic contain some of the most concentrated sources of FODMAPs. Fructans are the primary FODMAP type found in garlic.
Unless you have found that fructans are not a problematic FODMAP for you, eliminate all garlic while on the low-FODMAP diet.
Limiting garlic in your diet is especially challenging, as the food is commonly added to flavorings, broths, spice mixes, sauces, and gravies.
Despite being high in FODMAPs, garlic is gluten-free, and is associated with many health benefits.5 If you have successfully reintroduced garlic back into your diet and no intolerance is noted, feel free to include it in your diet.
4 ways to cook flavorful meals without consuming onion and garlic:
If your favorite home-cooked dish calls for garlic and onion, you don’t have to banish those flavors from your dinner table forever!
#1
Use Garlic Substitutes
Fresh garlic chives and the green tops of leeks are safe bets and add very similar flavors to your dishes! Find these ingredients in many asian markets, farmers markets, or easily grow them in a pot at home, or in your own garden.
Available in some parts of the U.S. in June and July, garlic scapes have also been shown to be well-tolerated by FODMAP-sensitive individuals. Additionally, Gourmend offers a Low-FODMAP Garlic Scape Powder that is a certified option for cooking, when used in moderate amounts. For adding a little zest to vegetables, soups, or meats sprinkle in about 1/4 tsp (per serving).
#2
Use Onion Substitutes
Add a burst of onion flavor to your cooking with:
- Leek tops
- Scallion/green onion tops
- Fresh and dried chives
- Asafoetida powder
Commonly used in Indian cooking and sold at Indian markets, asafoetida powder (also known as hing) can replace the flavor of onion. Asafoetida is a potent spice with a pungent scent, and a little goes a long way.
Do not just sprinkle asafoetida on top of your finished meal, as the resulting taste will be rather forward and unpleasant. To temper its bitterness and release the exotic flavor of this spice, add a pinch of asafoetida to hot oil or butter, mixing it into the spices that have already been added to the fat. After it is all mixed and dissolved, you can combine the mixture with your vegetables, meats, or rice.
At Gourmend, we’ve replaced the onions and garlic commonly found in off-the-shelf stocks with the green parts of leeks and scallions to produce chicken broth that lets you skip the onion, and still prepare and share delicious meals with your family.
#3
Use Infused Oils
Fructans are not soluble in oil, so the fructans in onions and garlic won’t leach out into the food you’re cooking... but the flavor will!
So how do you prepare stir-fries and other oil-based dishes with onions and garlic? Upgrade your meals by making your own onion or garlic-infused olive oil to cook with.
Heat oil in a frying pan and add a large slice of onion or a whole garlic clove to maximize the flavor. Be sure to remove the pieces before adding any other ingredients to the dish—including water!
The bacteria that causes botulism can grow well in infused oils. To prevent botulism, a dangerous bacterial poisoning, follow the CDC recommendation6 to enjoy your infused oil when it’s ready, refrigerating any leftovers immediately and discarding after a week at most.
#4
Use Other Herbs & Spices
Experiment with seasoning and cooking with herbs and spices that are garlic and onion-free. To infuse your meals with flavor, cook with low-FODMAP ingredients like:
- Lemon/lime juice and zest
- Herbs like thyme, basil, chives, parsley, lemongrass, dill, oregano, cilantro, rosemary and most others.
- Ginger, mustard seeds, sesame seeds, sumac, turmeric, chilis, coriander, cumin and many others.
Be aware: While most fresh and dried herbs and spices are carbohydrate-free (and therefore low-FODMAP) some IBS sufferers have noted intolerance with particularly spicy seasonings such as chili, which contains capsaicin and may aggravate IBS symptoms. Modify recipes accordingly and determine what works best for you.
The Takeaway:
Being prescribed a low-FODMAP diet to address FODMAP-sensitivity may leave you feeling that you have to compromise flavor to be healthy. But even if you can’t consume garlic and onions, your meals can still be extremely savory and flavorful!
Part 4 Proteins & Legumes
In this chapter, we'll go over:
- The high-FODMAP proteins and legumes you should avoid
- What to look for on labels
- How low-FODMAP meats, vegetarian proteins, legumes, and pulses can be part of a diet full of flavor and variety
Avoid high-FODMAP proteins and legumes, including:
- Sausages, hot dogs, and other processed meats (which are often flavored with garlic, onions, wheat, or a combination of many gut-aggravating FODMAPs)
- Broad (fava) beans, butter beans, baked beans, black-eyed peas, split peas, and soybeans
- Almonds, cashews, and pistachios
There are plenty of low-FODMAP proteins that are safe to eat, including:
Meat
- Beef
Including ground beef - Ham
Prosciutto, cold cuts, and other deli meats (as long as they have not been flavored or cured with onion or garlic powders or celery juice) - Lamb
- Pork
Poultry
- Chicken
- Duck
- Turkey
Fish & Seafood
- All fresh fish
- Canned tuna
- Crab
- Mussels
- Oysters
- Lobster
- Prawns
- Shrimp
Meat Substitutes
- Almond butter
- Macadamia nuts, peanuts, pine nuts, pecans and walnuts
- Peanut butter
- Sesame and sunflower seeds
- Tofu (firm), tempeh, and other soybean-based products
Be sure to check the labels:
- Stick with poultry, meat, and seafood that contain only salt (if anything) and are fructose and preservative-free.
- In the case of cold cuts and deli meats, be certain that no garlic, onions, honey, molasses, carrageenan, celery juice, or other high-FODMAP ingredients were added for seasoning.
- Tuna filets and canned tuna can be included in your low-FODMAP diet. Check the label of water-packaged tuna, however, as some brands use a combination of water and a potentially high-FODMAP broth.
Legumes & Pulses
Legumes and pulses can be a problematic food because they are naturally high in galactans, an oligosaccharide. But a flavorful, robust diet doesn’t have to be void of legumes!
Canned legumes, and legumes that have been boiled and drained have been shown to have less FODMAP content than their unprocessed counterparts. This is because the galactans in legumes seep out and dissolve into the water that they are cooked or canned in.
How to enjoy legumes while restricting FODMAP proteins:
- Choose jarred or canned legumes (well–drained and rinsed), such as canned lentils, which contain half the FODMAP level of those that are freshly boiled from their dried counterparts. That’s because more of the FODMAP content has had a chance to leach out into the can’s water during processing and storage.
- After cooking fresh legumes, always strain them to avoid consuming any FODMAP-saturated water. You might even try leaving them soaking in water in the refrigerator overnight and discarding that water, too, before eating.
- Eat small portions of legumes while on a low-FODMAP diet. The safest choices are lentils and chickpeas—but you can also enjoy very small amounts of other favorites like butter beans, kidney beans, canned pinto beans, black beans, adzuki beans, lima beans, and mung beans. To obtain the specific serving sizes of these beans, download the Monash University FODMAP Diet app.
Be aware that although canned legumes may have a reduced-FODMAP content, they can still be a significant FODMAP source. If you are sensitive to legumes and pulses, even in small quantities, consider relying on other low-FODMAP sources for protein.
The Takeaway:
With a substantial list of low-FODMAP proteins to choose from, you can replace flavor instead of sacrificing taste when mealtime comes around. Although it takes some initial effort to adapt your eating habits, the health benefits are worth the work!
Part 5 Wheat & Grains
In this chapter, we'll explain:
- What high-FODMAP grains and wheat-based foods should be restricted
- How to include corn and rice in your diet
- How to select whole-grain, low-FODMAP alternatives to wheat
Wheat, Amaranth, Barley, and Rye
Wheat is the primary source of FODMAPs in the Western diet. This is not because wheat is a concentrated FODMAP source, but rather because we consume this carbohydrate in large quantities.
In fact, wheat contains one of the lowest amounts of FODMAPs by weight. Wheat-based flavorings, thickeners, and foods that contain wheat as a minor ingredient are generally low-FODMAP. That said, anyone on the low-FODMAP diet should restrict wheat-based bread, breakfast cereals, biscuits, pasta, and pastries and select low-FODMAP, whole-grain alternatives.
In addition to wheat, limit your intake of high-FODMAP grains such as amaranth, barley, and rye, which can contain almost twice the number of FODMAPs as wheat.
Gluten Free vs Low FODMAP
Despite the fact that gluten and FODMAPs are present in many of the same foods, FODMAPs and gluten are not interchangeable.
Those diagnosed with celiac disease have an auto immune reaction to gluten,7 which is the protein found in barley, brewer’s yeast, rye, and wheat – those that have this disease cannot have any grains or products that contain gluten. Someone with a FODMAP sensitivity, on the other hand, suffers from a reaction to fructans, the specific carbohydrate type found in barley, rye, and wheat.
It is possible that individuals with celiac disease or non-celiac gluten sensitivity (gluten sensitivity) may have trouble digesting FODMAP carbohydrates as well. Provided that gluten ingestion has been ruled out as an issue, individuals with celiac disease or gluten sensitivity whose symptoms do not subside even after cutting out gluten may want to discuss trying the 3-step, low-FODMAP diet outlined in Part 2 above with their dietician, as some studies8 have shown this to be a help.
Corn
Sorbitol is the naturally occurring substance that makes corn sweet. When eaten as a vegetable in any beyond a small quantity, it contains enough sorbitol to be moderate in FODMAP levels.
The types of corn that are meant to be ground into cornmeal (corn flour, masa harina, or masarepa) are lower in the FODMAP sorbitol and higher in starch.
Since starch is not a FODMAP, arepas, corn tortillas, corn pasta, grits, polenta, pupusas, tamales, and other ground-corn based foods can be consumed by individuals on a low-FODMAP diet.
Be aware: Be certain that other high-FODMAP ingredients have not been added before including any of the ground-corn foods mentioned above in your diet.
Rice
Brown and white rice are both low in FODMAPs, so experiment with recipes using these low-FODMAP ingredients.
When cooking rice, do not use broths or stocks that contain garlic or onion. Avoid preparing rice with coconut water as well. Instead, stick to rice cooked with water or a low FODMAP chicken broth and a dash of garlic scape powder for extra flavor.
Alternative Low-FODMAP Grains
In addition to rice, select whole-grain, low-FODMAP alternatives like buckwheat, millet, oats, cornmeal (e.g. polenta), quinoa, and tapioca-based foods.
Sprouted Grains
Some studies9 suggest that the FODMAP content of the grains barley, rye, and wheat may be reduced through sprouting. To test sprouting’s effectiveness, eat a small amount of the sprouted grain and monitor your tolerance.
Sourdough Breads
Well-made sourdough bread can be low FODMAP, since there is a fermentation step involved in the process of making it. This fermentation step has been shown to reduce the fructan content by over 70%10, because the yeasts ferment the fructans during the process of leavening bread.
Traditional sourdough breads made from wheat and spelt flours are low FODMAP because of these decreased fructan levels. Dough should proof (i.e. the process of leaving it to rise) for 1-2 days, using a starter that has fermented for at least 12 hours, to achieve high-quality, FODMAP-safe bread.
Although sourdough bread can be found on supermarket shelves, making your own or buying bread from a trusted artisan or local baker you can talk with is a great way to ensure that this slow fermentation process has occurred.
The Takeaway:
Although wheat is prevalent in everything from bread and cereal to pasta and baked goods, this source of FODMAPs can be avoided by selecting well-made sourdough bread, ground-corn based pasta, brown and white rice alternatives, buckwheat, oats, polenta, quinoa, and other wheat-free alternatives.
Part 6 Fruits & Vegetables
In this chapter, we'll explain:
- The difference between fructose and fructans
- What makes certain fruits and vegetables low in FODMAPs
- When and how to include high-FODMAP fruits and veggies into your diet
Fruit
Although they are both FODMAPS, fructose is not the same as fructans.
Fructose is a fruit sugar naturally found in honey, vine and tree fruits, and most root vegetables. Fructans are a type of carbohydrate made by a chain of fructose molecules strung together.
All fruit naturally contains fructose, and some fruit contains glucose.
Glucose is an important non-FODMAP sugar, as it helps your body absorb fructose.
Although glucose is not a FODMAP, fruit that contains more fructose than glucose is considered high-FODMAP.
In addition to fruit that contains high amounts of excess fructose, fruit that is high in fructans and / or contains high amounts of sorbitol should be avoided, as these have also been designated as high-FODMAP.
Limit these high-FODMAP fruits:
- Apricots
- Apples
- Avocados
- Bananas
(ripe) - Blackberries
- Cherries
- Dates
- Figs
- Grapefruit
- Mango
- Nectarines
- Peaches
- Pears
- Plums
- Raisin
- Watermelon
Enjoy these low-FODMAP fruits*:
- Bananas
(unripe) - Blueberries
- Cantaloupe
- Clementines
- Coconut
- Dragonfruit
- Honeydew Melon
- Kiwi fruit
- Lemon
- Lime
- Oranges
- Papaya
- Passionfruit
- Pineapple
- Raspberries
- Rhubarb
- Starfruit
- Strawberries
*To obtain the specific serving sizes of these foods, download the Monash University FODMAP Diet app.
Vegetables
Vegetables contain the most diverse range of FODMAPs and several vegetables actually contain more than one FODMAP type. Swap out high-FODMAP vegetables for low-FODMAP choices.
Skip these high-FODMAP vegetables:
- Artichokes
- Asparagus
- Beans
- Brussels sprouts
- Butternut squash
- Cauliflower
- Celery
- Corn
- Garlic
- Mushrooms
(except oyster which are low!) - Onions
- Peas
Enjoy these low-FODMAP vegetables:
- Alfalfa
- Arugula
- Bamboo shoots
- Bean sprout
- Bok Choy
- Broccoli
(as few stems as possible) - Cabbage
- Carrots
- Cucumbers
- Chili peppers
- Bell peppers
(green color) - Eggplant
- Endive
- Fennel
- Ginger
- Green beans
- Leek tops
(green parts) - Lettuce
- Kale
- Okra
- Olives
- Potatoes
- Radishes
- Scallion tops
(green parts) - Spinach
- Summer Squash
- Tomatoes
- Turnips
*To obtain the specific serving sizes of these foods, download the Monash University FODMAP Diet app.
The Takeaway:
At no point during the low-FODMAP diet should you cut out eating fruit and vegetables entirely, since both are an important part of a wholesome diet. With so many low-FODMAP options to choose from, it’s easy to eat the recommended servings of fruits and veggies every day.
Part 7 Dairy
In this chapter, we'll explain:
- The high-FODMAP dairy products that should be removed from your diet
- The difference between traditional yogurt and Greek yogurt
- Low-FODMAP dairy items and dairy alternatives that are safe to eat
Although the FODMAP lactose is found primarily in dairy products, an extensive number of dairy products are naturally low in lactose. That’s because many dairy products, like most hard and matured cheeses, lose their lactose during the cheesemaking process.
The following high-FODMAP dairy products should be replaced with lactose free versions:
*Traditional vs. Greek Yogurt
Yogurt is produced when the bacteria Lactobacillus bulgaricus and Streptococcus thermophilus are added to milk, causing the milk to ferment.
Greek yogurt is the result of straining yogurt after this fermentation process, which removes the watery whey that contains much of the lactose and yields a yogurt that is higher in fat and lower in lactose. Typically, Greek yogurt’s lactose content is 5 to 8 grams per 6 ounce serving11, making it more likely to be FODMAP safe.
In addition there are plenty of other low-FODMAP dairy items and dairy alternatives that you can eat, including:
Cheeses
- Safe at about 1 slice or 40 grams (not flavored with onion or garlic), including: Brie, Cheddar, Colby, Goat, Havarti, Mozzarella, Monterey Jack, Parmesan & Swiss
Butter
- Butter is made of milk, but its high-fat composition makes it naturally low in lactose and FODMAP safe!
Milk Alternatives
- Lactose-free milk
- Almond milk
- Coconut milk
- Rice milk
A Word on Lactose Intolerance
If you are an IBS sufferer on the low-FODMAP diet, consult with your doctor or dietitian to determine if you are also lactose intolerant. It’s possible that you may only need to restrict lactose if you are lactose intolerant.
According to research, regularly consuming small portions of dairy throughout the day may minimize your intolerance of the FODMAP lactose.12 Rather than eating dairy alone, using dairy as an ingredient in a dish you prepare may also increase your tolerance of lactose
If you are restricting lactose, there are several products that contain lactase, an enzyme that can help you better digest lactose. Available from most pharmacies, lactase tablets or drops are an enzyme supplement that may help some people who are lactose intolerant better digest lactose.
The Takeaway:
It’s true that the FODMAP lactose is found primarily in dairy products, but an extensive number of dairy products are naturally low in lactose. Enjoy a wide variety of cheese and other dairy products low in FODMAPs while on the low–FODMAP diet.
Part 8 Beverages & Sweeteners
In this chapter, we'll look at:
- High-FODMAP beverages and sweeteners to avoid
- What low-FODMAP sweeteners and beverages to select
- Why beverages with low-FODMAP ingredients can still be high FODMAP
Beverages
Beverages are a source of significant FODMAPs, even if the beverage was not made from blatantly high-FODMAP ingredients.
Some beverages are naturally high in FODMAPs, while additives and sweeteners may spike the FODMAP levels of otherwise low-FODMAP beverages.
Skip these high-FODMAP beverages:
- Sodas containing high fructose corn syrup (HFCS)
- Juices containing HFCS, agave or honey
- Strong herbal tea
- Strong black tea
- Strong chai tea
- Strong dandelion tea
- Fennel tea
- Chamomile tea
- Oolong tea
- Coconut water
- Whey protein and milk-based health shakes
- Most fruit juices
(apple, orange, mango, etc)
Enjoy these low-FODMAP beverages:
- White and green tea
- Peppermint tea
- Weak chai tea
- Weak black and herbal teas
(strong teas contain moderate amounts of fructans) - Pure hot chocolate
(made from cacao powder and sweetened with regular sugar)
- Black coffee
- V8® vegetable blend juice
- Tomato juice
- Cranberry juice (pure, without high fructose, apple juice and pear juice)
- Flavored waters or lemonade
(as long as flavored with basic table sugar / sucrose) - Dry wines, beer & spirits
(see notes below)
A note on dairy:
Adding cow’s milk, dairy creamer, or soy milk to your coffee can alter its FODMAP content. Although coffee is low in FODMAPs, a serving size of coffee containing milk or creamer may contain high amounts of the Oligos-GOS or high amounts of lactose. If you malabsorb lactose, refrain from adding dairy to your coffee.
A note on caffeine:
Drinking caffeinated beverages may cause digestive distress in some people because caffeine is a bowel stimulant. Despite being low-FODMAP, coffee and tea containing caffeine have been linked to IBS symptoms. It’s important that you work with a registered dietitian to evaluate your personal experience with caffeine and modify your diet accordingly. Your dietitian may recommend that you transition to decaffeinated beverages.
What about juice from low-FODMAP fruit?
Although juices may be consumed, they should not be consumed in large quantities, even if associated with low-FODMAP fruits. Aim for quantities of less than half a cup.
That's because beverages made with low-FODMAP ingredients can still be high FODMAP.
Why? It's all about quantity! Juices like orange juice are generally made from oranges, which are low FODMAP, but orange juice is still considered high FODMAP once you have too much.
While oranges are low FODMAP, they do contain fructose, as well as glucose and sucrose. Glucose is an important non-FODMAP sugar, as it helps your body absorb fructose.
Although glucose is not a FODMAP, food and beverages that have more fructose than glucose are considered high FODMAP. Because of the amount of oranges used to make orange juice, an 8-ounce glass of juice has substantially more fructose than one orange, enough to make that glass high FODMAP.
What about alcohol?
Generally, alcohol is an irritant for IBS-prone individuals. Avoid digestive distress by consuming alcohol with low FODMAP food, rather than on an empty stomach.
- Although it is typically made from wheat, beer is actually on the list of safe beverages for those following a low-FODMAP diet. The recommended serving size is 12 ounces or less.
- When it comes to wine, be careful which type you are drinking… and how much! Limit marsalas, ports, and most dessert wines, which are high in the FODMAP fructose. However, most red, white, and sparkling wines are a good choice. 1 glass of those drier wines, for example, are typically low FODMAP.
- Additionally, one drink containing gin, vodka, or whiskey is FODMAP safe as well.
What about kombucha tea?
Monash University FODMAP researchers have tested the FODMAP content of kombucha13 and found some types to be high FODMAP. High-FODMAP kombuchas tend to be those that are flavored, causing adverse gastrointestinal reactions to the specific ingredients that are added.
In addition to reactions to flavoring, another factor to consider is that some individuals may benefit from kombucha’s good bacteria. Others may already have too much of that specific bacteria in their gut, so kombucha could cause a bacteria overgrowth.
When following the low FODMAP diet, limit consumption of kombucha to less than a glass to prevent IBS symptoms.
What about apple cider vinegar?
It’s true that apples are high in FODMAPs, but when it comes to apple cider vinegar, the double fermentation process decreases the high levels of fructose and sorbitol found in apples, making levels safe enough to be considered low FODMAP.
According to Monash University’s low-FODMAP app, 2 tablespoons or less of apple cider vinegar is a safe serving for anyone adhering to a low-FODMAP diet. Consuming a serving size of unfiltered apple cider vinegar can also have health benefits, including destroying harmful bacteria and preventing their growth.
Sweeteners
Sweeteners can be another hidden source of FODMAPs, and adding sweeteners to an otherwise low-FODMAP food can raise its overall FODMAP content. Below is a list of high-FODMAP sweeteners to avoid, both alone, and when listed in any product’s ingredients.
Skip these high-FODMAP sweeteners:
- Agave
- Honey
- High fructose corn syrup (HFCS)
- Molasses
- Inulin
- Isomalt
- Maltitol
- Mannitol
- Sorbitol
- Xylitol
Select low-FODMAP sweeteners:
When selecting low-FODMAP sweeteners, stick with standard table sugar (often noted as sucrose, sucralose or glucose on labels) and maple syrup.
Many artificial sweeteners like acesulfame K, aspartame, saccharine, and stevia are low FODMAP, but you may wish to avoid these for other health reasons.
A warning about sweeteners in beverages:
Carbonated drinks often contain high-FODMAP sweeteners like high fructose corn syrup or agave. Drinks sweetened with real sugar (sugar cane, sucrose, sucralose) should be okay for most people, in moderation.
Are simple white and brown sugars a safe choice?
Sugar contains fructose and glucose in equal amounts. According to Monash University, it is safe to use as a sweetener for baking, or mixed in a drink, since sugar does not meet the definition of a FODMAP. Dark chocolate, white, brown, and raw sugar are all safe choices.
Check the Ingredients
In the case of sweeteners and beverages, some are very obviously high-FODMAP (here’s looking at you high fructose corn syrup!), while the FODMAP content of others is not so apparent. Many beverages, sweeteners, condiments, and even fruit juices can be a hidden source of FODMAPs.
With that in mind, it’s wise to always check the ingredients list on packaged foods and bottled beverages.
- Keep an eye out for apples, apple juice, or mango juice that may be used in beverages, spiking FODMAP levels.
- Check the ingredients listed on beverages and packaged foods to ensure that you avoid high-FODMAP sweeteners.
- Check the ingredient lists of mints, gum, and any food product that is labeled as “sugar free” for high-FODMAP sweeteners like sorbitol, maltito, and xylitol.
The Takeaway:
The high-FODMAP world of beverages and sweeteners can be tricky to navigate, but there are plenty of low-FODMAP options out there, and they won’t aggravate your stomach either. If you are diligent about checking labels and you know what to look for, you can make low-FODMAP choices. You can even include a glass of wine or a beer with your meal.
Part 9 Cooking Nutritious, Flavorful Meals
In this chapter, you’ll learn how to reclaim the full flavor of home cooking with:
- Low-FODMAP ingredients you can stock your kitchen with
- Tips for cooking low-FODMAP meals that are nutritious
- Our favorite low-FODMAP recipes for savory, healthy eating
Stock your kitchen with low-FODMAP ingredients
The low-FODMAP diet is one that limits certain food ingredients and is personalized to your sensitivities. The diet does not completely eliminate all foods that contain FODMAPs, however, so you don't have to settle for cooking a handful of bland dishes.
Here are the steps to stocking your kitchen with low-FODMAP food:
- Remove all ingredients that you know can aggravate your stomach from pantries and the fridge.
- Download and print out this convenient FODMAP-Friendly Shopping List to refer to when cooking and shopping during the week.
- Use the “Notes” section on the card to list FODMAPs that you and your dietician have determined safe, even in small quantities.
- Finally, add any other desired ingredients to the FODMAP-Friendly side of the card, and get shopping!
Another helpful shopping companion is Fig (Food is Good) It's an app that helps you find new food that matches all of your dietary needs.
Whether you’re Low FODMAP, have food allergies, or simply want to cut out certain ingredients, Fig has you covered. No more restrictions. Only options. We recommend FIG as a great resource in combination with the Monash Low FODMAP App.
From comfort foods to gourmet meals, you can cook a variety of flavorful meals if you stock your pantry and fridge with the staples listed below!
Herbs
For a nourishing way to add flavor to any low-FODMAP dish, choose dried or fresh herbs like basil, coriander, parsley, rosemary, tarragon, and thyme. To have fresh herbs on hand, you can even grow your own.
Spices
To add some kick to your meals, select cumin, coriander, ginger, turmeric, or other classic spices that have been tested and approved as low FODMAP. Don’t forget about cooking with small amounts of Asafoetida powder or our own garlic scape powder either!
Stock your kitchen cupboards with jars of spices like cinnamon, chili powder, smoked paprika, and fennel seeds. If you need to spice up a bland dish, try cooking with finely chopped lemongrass, or even fresh fennel leaves (without the bulb).
Citrus
Citrus is the new garlic. Although it may not offer the same flavor, it can provide an aromatic bite just like garlic does.
Use grated lemon zest like you would garlic in hummus, chicken marinades, and spice mixes.
Ginger
Add fresh ginger to your grocery list and achieve a spicy aroma by creating curries and stir-fries. Store a few cups of thinly sliced ginger in your freezer for easy meals on busy weeknights.
Sliced ginger makes a good base for risottos, stir-fries, stews, soups, and other popular recipes as well.
Alliums’ Green Parts
Alliums are a bulbous plant and include cultivated chives, leek, garlic, onion, scallion, and shallot. And not all alliums are taboo!
For the earthy sweetness of onion without the FODMAPs, substitute onions with the green parts of chives or scallions. You can also swap out onions for green leek tops. For maximal flavor and texture, sauté thin slices over low heat in olive oil.
If your meal is lacking depth after cutting out onions, swiss chard stems also make a tasty substitute when sautéed.
Condiments
Go ahead and cook with sauces and condiments, as long as they are free of onion, garlic or high-FODMAP sweeteners as discussed in the last chapter. The following are good low-FODMAP staples to keep in your kitchen and fridge:
- Fish sauce
- Soy sauce
- Ketchup
(very small amounts) - Mustard
- Mayonnaise
- Worcestershire sauce
- Wasabi
- Green habanero sauce
- Sriracha hot sauce
- Plain tomato paste
- Plain tomato sauce
*To obtain the specific serving sizes, download the Monash University FODMAP Diet app.
A note on ketchup:
Ketchup is a condiment that can be high in FODMAPs based on its fructan content. Many ketchup brands also contain high fructose corn syrup (HFCS) as well, which may cause confusion over whether ketchup should be part of a low-FODMAP diet.
Whether ketchup is made with high fructose corn syrup or with sucrose, it is suggested to enjoy less than 2 teaspoons. Small portions are key when enjoying ketchup!
A note on mustard:
Mustard is a tasty condiment that you can continue to enjoy when preparing low FODMAP meals. A serving size of 1 tablespoon is low in FODMAPs and should be well-tolerated. Carefully read the ingredients on the mustard label, however, as some manufacturers may add garlic or onion as a spice or natural flavor. If onion or garlic have been added, avoid that variety and opt for a version of the tangy condiment that is made with only dry mustard powder or ground mustard and water or vinegar.
Dressings
For salads, try making your own dressing using coconut oil, olive oil, sesame oil with vinegar (apple cider, balsamic, or red wine), lemon, or a dash of dijon mustard plus some salt, pepper and a sprinkle of chives or other herbs.
As always, check the labels to catch any hidden, high-FODMAP ingredients.
3 tips for cooking low-FODMAP, nutritious meals:
After you’ve worked with your dietician to determine which FODMAPs are personal triggers, you may have to make modifications to the recipes you love to cook and share with your family.
With homemade stocks, low FODMAP infused oils, and a little creativity, you can put flavorful meals back on the dinner menu!
#1
Infuse Your Own Oil
The fructans in garlic and onion are often a source of IBS symptoms. Fortunately for low-FODMAP foodies, garlic is not oil-soluble, which means that by infusing oil with garlic, you get all of the aromatic flavor and none of the FODMAPs. To prevent botulism, follow the CDC recommendation14 to enjoy any refrigerated leftovers within a few days.
Garlic-flavored oil and garlic-infused oil are not the same!
Garlic-infused oils are made by letting garlic cloves, and garlic cloves alone, marinate in heated oil. The garlic cloves are completely removed once the desired flavor is achieved. Garlic-flavored oils have dried, fresh, or roasted pieces of garlic floating in the bottle. These pieces are the source of the flavor… And they are the reason garlic-flavored oil can be high FODMAP. If an oil contains garlic pieces, garlic salt, or garlic powder, then it has the potential to trigger gastrointestinal issues.
Always check the ingredients before cooking with any product that is labeled as garlic oil, garlic essential oil, garlic essence or garlic-flavored.
#2
Use Green Chives, Leek Tops & Scallion Tops
If your favorite recipes call for onion or garlic powder, Gourmend's certified low FODMAP garlic scape powder could be the alternative your stomach has been waiting for. Furthermore, to reclaim the robust taste of cooking with garlic or onions, slice raw scallion tops and/or chives and add a handful or two to pasta dishes, stews, salsas, and any recipe that gets its richness from alliums.
#3
Grow Your Own Flavor
To have onion and garlic flavoring at your fingertips, grow your own leeks, green onions, chives, or garlic chives from seeds. Once the plants are full-grown, just snip off whatever amount of the green part that you need, and toss it into any meal that calls for onions. The plant will continue to grow in the soil and you’ll be able to add a burst of onion flavor to any dish.
The Takeaway:
If you can’t cook with onion, garlic, and other high-FODMAP ingredients, don’t think of your kitchen as empty. Think of it as a blank slate for tapping into your creativity as a cook, putting a delicious twist on favorite family recipes, and discovering new dishes that will be a big hit.
Part 10 Dining Out
Being on the low-FODMAP diet doesn’t mean you have to cancel all your dinner reservations. In this chapter, you’ll discover:
- How you can identify a few low-FODMAP options and dine out with confidence
- What to eat on the go when traveling
- Tips for foods you should and should not be eating, whether you’re at a party or a restaurant
Dining Out:
Before dining out, get familiar with the restaurant’s menu. Most dining establishments and cafes will post their menu online, so you can visit their website for ideas on FODMAP-safe dishes they offer.
If this is not the case, call to confirm that they serve dishes to accommodate your needs, or if you can order meals that can be easily altered. Once you identify a few low-FODMAP options, you can dine out with confidence.
And don’t leave home without your FODMAP Friendly Dining Card. You can hand the card to your server to take the guesswork out of communicating your dietary restrictions and ensuring your meal doesn't contain any of your IBS triggers.
When ordering, ask for sauces and dressing on the side, pass on croutons for your salad, and substitute noodles with rice.
If a dish would require that the chef make more than three changes for you, it’s best to be polite and order a different dish. But don’t hesitate to send the dish back if a change was not made as you requested.
Traveling for vacation or a business trip?
Pack your FODMAP-Friendly Dining Card and non-perishable low-FODMAP foods for on the go snacking, including:
- Low-FODMAP nuts and seeds
- Gluten, garlic & onion-free bars, pretzels, and cereals
- Plain chips (corn or potato)
- Plain popcorn
- Plain rice cakes
- Individual packets of peanut butter
Going to a party or cookout?
Even if it isn't a potluck, you can ask the host if you can prepare a few low-FODMAP dishes to share. The other guests might be surprised to find that FODMAP-friendly food can be so delicious!
Even low-FODMAP alcoholic beverages can aggravate the digestive tract, so stick to the Monash University low FODMAP Diet App’s recommended portions for wine, beer, gin, and vodka.
Gastrointestinal symptoms may make going out to eat or attending a party stressful. But one of the best things you can do to calm your gut other than stick to your low-FODMAP diet is to relax.
The Takeaway:
With a little preparation and some good communication, you can cook in, eat on the go, dine out, and live life again!
Part 11 Advice & Support
This chapter will provide you with resources to make the process easier, including:
- Facebook groups and apps offering support for those of us living low FODMAP
- Sources of helpful information and advice, such as diet professionals’ books and blogs
- Additional online support, diet plans, and recipes from nutrition experts
Following a low-FODMAP diet may seem overwhelming, but remember that this is a process. It will take time to heal your gut, identify foods that you are personally sensitive to, and incorporate low FODMAP ingredients into recipes to reclaim your favorite flavors.
The following are some of the diet experts, resources, websites, and books that support a FODMAP-friendly diet:
Nutritionists & Registered Dietitians
Monash University has compiled a list of FODMAP trained dietitians and Patsy Catsos, MS, RDN, LD has compiled a Google Spreadsheet of FODMAP dietitians.
Favorite Blogs
Monash Blog
As the official blog of Monash University, one of the world’s top universities as well as the institution that originated FODMAP research, this blog features posts by research dietitians, chefs, healthcare professionals, and other nutrition experts.
FODMAP Everyday
Highly qualified and experienced RDNs, complementary health practitioners, and recipe developers bring appropriate guidance and information to help readers successfully navigate the journey towards improved health.
A Little Bit Yummy
Find low-FODMAP recipes and resources approved by dietitians. The blog is intended to help others gain symptom control through delicious low-FODMAP meal plans.
FODMAP Life
This blog focuses on the low-FODMAP diet, as well as other natural ways to help care for the body and mind.
For a Digestive Peace of Mind
Run by Kate Scarlata, a registered dietitian and low-FODMAP diet expert, this blog is full of recipes and tips.
The IBS-Free Digest
Run by Patsy Catsos, a registered dietitian and low FODMAP expert, this blog is full of tips on living with a low-FODMAP diet.
Favorite Books
Facebook Groups
Conclusion
It takes time to learn how to follow a low–FODMAP diet for improved gut health, but it can be done!
With time, creativity, and support, you can eat meals that are nutritious and delicious while limiting high–FODMAP ingredients. You CAN take control of digestive distress and be free to be friends with food again!
The information in this guide is not intended to replace medical treatment and counsel that your health care provider offers. It is intended to educate and supplement personalized medical advice, while providing support at all stages of the low-FODMAP diet experience. Keep in mind that we offer these resources and suggestions for support, education and guidance only. Use them to complement consultations with a registered dietitian.
- Marsh A, Eslick EM, Eslick GD. Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr. 2016 Apr;55(3):897-906. doi: 10.1007/s00394-015-0922-1. Epub 2015 May 17. Review. PubMed PMID: 25982757.
- Zhan YL, Zhan YA, Dai SX. Is a low FODMAP diet beneficial for patients with inflammatory bowel disease? A meta-analysis and systematic review. Clin Nutr. 2018 Feb;37(1):123-129. doi: 10.1016/j.clnu.2017.05.019. Epub 2017 May 24. PubMed PMID: 28587774.
- Ong DK, Mitchell SB, Barrett JS, Shepherd SJ, Irving PM, Biesiekierski JR, Smith S, Gibson PR, Muir JG. Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol. 2010 Aug;25(8):1366-73. doi: 10.1111/j.1440-1746.2010.06370.x. PubMed PMID: 20659225.
- Shaukat A, Levitt MD, Taylor BC, MacDonald R, Shamliyan TA, Kane RL, Wilt TJ. Systematic review: effective management strategies for lactose intolerance. Ann Intern Med. 2010 Jun 15;152(12):797-803. doi: 10.7326/0003-4819-152-12-201006150-00241. Epub 2010 Apr 19. Review. PubMed PMID: 20404262.
- Newman, Tim. “What are the benefits of garlic?” medicalnewstoday.com. 18 Aug. 2017.
- "Prevention: Many cases of botulism are preventable." cdc.gov. 7 Jun. 2019.
- De Re V, Magris R, Cannizzaro R. New Insights into the Pathogenesis of Celiac Disease. Front Med (Lausanne). 2017;4:137. doi: 10.3389/fmed.2017.00137. eCollection 2017. Review. PubMed PMID: 28913337; PubMed Central PMCID: PMC5583152.
- Roncoroni L, Bascuñán KA, Doneda L, Scricciolo A, Lombardo V, Branchi F, Ferretti F, Dell'Osso B, Montanari V, Bardella MT, Elli L. A Low FODMAP Gluten-Free Diet Improves Functional Gastrointestinal Disorders and Overall Mental Health of Celiac Disease Patients: A Randomized Controlled Trial. Nutrients. 2018 Aug 4;10(8). doi: 10.3390/nu10081023. PubMed PMID: 30081576; PubMed Central PMCID: PMC6115770.
- Tuck, Caroline, MD. "Sprouting – does it reduce the FODMAP content of foods?". monashfodmap.com. 28 Mar. 2017.
- Verspreet J, Dornez E, Ende W, Delcour J, Courtin, C. "Cereal grain fructans: Structure, variability and potential health effects". Trends in Food Science & Technology. 43(1), 32-42
- Shaukat A, Levitt MD, Taylor BC, MacDonald R, Shamliyan TA, Kane RL, Wilt TJ. Systematic review: effective management strategies for lactose intolerance. Ann Intern Med. 2010 Jun 15;152(12):797-803. doi: 10.7326/0003-4819-152-12-201006150-00241. Epub 2010 Apr 19. Review. PubMed PMID: 20404262.
- Shaukat A, Levitt MD, Taylor BC, MacDonald R, Shamliyan TA, Kane RL, Wilt TJ. Systematic review: effective management strategies for lactose intolerance. Ann Intern Med. 2010 Jun 15;152(12):797-803. doi: 10.7326/0003-4819-152-12-201006150-00241. Epub 2010 Apr 19. Review. PubMed PMID: 20404262.
- Webber, Shirley. "Fermented drinks and the low FODMAP diet". monashfodmap.com. 28 Feb. 2017.
- "Prevention: Many cases of botulism are preventable." cdc.gov. 7 Jun. 2019.